알라딘: [전자책] 몸은 기억한다[eBook] 몸은 기억한다 - 트라우마가 남긴 흔적들
베셀 반 데어 콜크 (지은이),제효영 (옮긴이),김현수 (감수)
을유문화사2021-02-18
원제 : The Body Keeps the Score
===
책소개
뉴욕 타임스 베스트셀러, 아마존 베스트셀러, 미디어 호평 도서. 수십 년간 외상 후 스트레스 장애 분야를 연구해 온 세계적인 권위자 베셀 반 데어 콜크의 노작으로, ‘트라우마에 대한 현대의 고전’이라 인정받고 있는 『몸은 기억한다』 개정판이 을유문화사에서 출간됐다.
이 책은 트라우마 장애를 안고 있는 환자를 어떻게 바라봐야 할지부터 관련 연구의 발달 과정, 치료 방법, 우리 사회에 미치는 파장까지 총 망라하고 있어 관계자들은 트라우마와 관련해 당분간 이 이상의 책은 나오기 어려울 것으로 보고 있다.
『몸은 기억한다』는 트라우마로부터의 치유 없이 성장과 성과 속에서 내달려 온 현대인의 삶 속에 있는 트라우마를 이해하고 치유하면서 우리 사회를 더 건강하게 하기 위한 출발점에 놓일 책이다. 본 개정판은 문장을 이해하기 쉽게 다듬고, 도판과 각주를 추가하여 더 편하게 읽을 수 있도록 했다.
목차
감수 및 추천의 말
이 책에 대한 찬사
여는 글 | 트라우마와의 대면
1부 트라우마의 재발견
1장 베트남전 참전 군인들이 알게 해 준 교훈
2장 마음과 뇌의 이해, 그 혁신적 변화
3장 뇌 속을 들여다보다: 신경과학의 혁명
2부 트라우마 상태의 뇌
4장 필사적인 도주: 생존의 해부
5장 신체와 뇌의 유대
6장 몸을 잃으면 자기self를 잃는다
3부 아이들의 마음
7장 애착과 조율: 동일한 파장을 일으키다
8장 관계의 덫: 학대와 방임의 대가
9장 사랑과는 거리가 먼
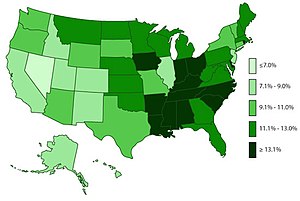
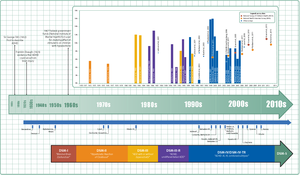
10장 발달 과정의 트라우마: 숨겨진 유행병
4부 트라우마의 흔적
11장 비밀의 발견: 트라우마 기억의 문제점
12장 참을 수 없는 기억의 무거움
5부 회복으로 가는 길
13장 트라우마로부터의 회복: 트라우마의 치유
14장 언어, 기적이자 고통
15장 과거를 떠나보내는 방법: 안구 운동 민감소실 및 재처리 요법EMDR
16장 내 몸에서 살아가는 법을 배우다: 요가
17장 조각 맞추기: 나를 리드하는 기술
18장 틈새 메우기: 새로운 구조 만들기
19장 뇌 회로의 재연결: 뉴로피드백
20장 잃어버린 목소리 찾기: 공동체의 리듬, 연극 치료
닫는 글 | 선택 앞에서
감사의 글
부록 | 트라우마 발달 장애 진단 기준에 관한 합의안
참고 자료
더 읽을거리
주석
찾아보기
접기
책속에서
첫문장
내가 열두 살이던 1975년, 유난히 춥고 하늘이 온통 구름으로 뒤덮였던 그 겨울날부터 나는 지금 이 모습이 되었다.
P. 62 의사들이 환자들의 증상을 열의 없이 논의하는 모습이나 환자를 자살로 몰고 가는 생각과 자해 행동을 이야기하면서 그 절망과 무기력감의 원인을 파악하는 대신 행동을 관리하는 일에 더 많은 시간을 쓴다는 사실을 알고 나는 자주 놀라곤 했다. 또한 의사들이 환자들이 이룬 성과와 그들이 가진 열망, 마음을 쓰고 사랑하는 대상이나 증오하는 ... 더보기
P. 241 어린 메릴린은 자신을 없애는 방법을 택했다. 침실 밖 복도에서 아빠가 걸어오는 발소리가 들리면, 메릴린은 ‘머리를 구름 속에 넣어’ 버렸다. 비슷한 일을 겪은 다른 환자 한 명이 직접 그림을 그려서 그 방식을 설명해 준 적이 있다. 아버지가 손을 대기 시작하면 그녀 역시 자신을 사라지게 만들었다. 천장을 지나 하늘로 붕 떠올라서 ... 더보기
P. 343~346 셋째 아이를 출산한 직후, 낸시는 복강경 난관결찰술을 받았다. 보통 외래 수술로 많이 실시되는 이 수술은 임신이 되지 않도록 난관을 소작하는 수술이다. 그런데 낸시는 수술 당일 마취가 충분히 되지 않아서, 수술이 시작된 후 곧 깨어나 그 상태로 수술이 거의 끝날 때까지 있어야 했다. ‘얕은 잠’ 혹은 ‘꿈을 꾸는’ 것 같았다고 설... 더보기
P. 478~479 집착, 충동, 공황 발작, 자기 파괴적인 행동 등 정신의학적으로 문제가 있다고 분류되는 행동들은 자기방어 전략에서 시작된 경우가 많다. 이와 같은 방식으로 트라우마에 적응하면, 의료 보건 전문가들이나 환자 자신도 완전한 회복이 너무 멀게만 느껴질 만큼 정상적인 기능에 심각한 악영향을 줄 수 있다. 그러나 그러한 증상을 영원히 해결... 더보기
트라우마 외상에 대해 다루는 것은 단지 트라우마만 다루어 주는 것이 아니라 환자와 함께 견디고 안전한 느낌을 줄 수 있는 사람, 대상, 환경을 만들어 가는 과정이며, 환자가 살아남기 위하여 몰두한 노력을 경외하는 것으로부터 출발해야 한다. - hjlee723
더보기
저자 및 역자소개
베셀 반 데어 콜크 (Bessel Van Der Kolk, M.D.) (지은이)
저자파일
신간알리미 신청
의학 박사로, 1970년대부터 외상 후 스트레스 장애(PTSD)를 연구해 온 권위자이자 세계적인 학자다. 하버드 의과대학에서 정신의학을 공부하고 매사추세츠 정신건강 센터에서 정신과 전문의 교육을 받았다. 보스턴 주립병원에서 근무하다가 보훈병원에서 일하며 참전 군인들에 관해 연구한 것이 외상 후 스트레스 장애에 대한 본격적인 연구의 시작이 됐다. 1982년 매사추세츠 정신건강 센터에서 정신약리학을 가르쳤고, 1980년대 중반에 트라우마 센터를 설립했다. PTSD가 뇌에 일으킨 변화를 뇌 신경 영상으로 조사한 최초의 연구에 참여했는데, 이 연구에서 밝혀진 결과는 트라우마 스트레스의 새로운 치료법이 탄생하는 데 중요한 계기가 되었다. 또한 신경 생물학, 뇌 과학 등 다양한 분야와 다각도로 연계해 여러 가지 성과를 이루어 내며 트라우마가 마음과 뇌, 몸의 발달에 끼치는 영향에 관한 광범위한 연구 결과를 발표해 왔고, 특히 정신적 해리와 경계성 인격 장애, 자해를 비롯한 다양한 문제와 트라우마의 연관성을 밝혀냈다. 그리고 트라우마가 발달 과정에 끼치는 영향을 연구하며 외상 후 스트레스 장애 치료에 요가나 뉴로피드백, EMDR, 연극 치료 등을 활용하는 방안을 연구해 그런 치료법들이 뇌에 변화를 일으켜 기능을 향상시킬 수 있다는 사실을 입증했다. 국제 트라우마 스트레스 연구회의 대표직을 역임했고, 현재 보스턴 의과 대학에 정신의학과 교수로 재직 중이며, 매사추세츠 주 브룩클린의 정의자원연구소 내 트라우마 센터에서 의학 책임자, 국립 아동 트라우마 스트레스 센터 소속 복합 트라우마 네트워크의 총책임자를 맡고 있다. 미국 전역의 대학교와 병원에서 강의를 해 왔고 유럽, 아프리카, 러시아, 오스트레일리아, 이스라엘, 중국, 브라질, 일본 등 여러 나라에서 강연했다. 또한 알코올과 약물 중독에 시달리는 트라우마 환자 치료 시설(The Meadows)의 선임연구원으로 치료사들에게 전문적인 지식을 제공하고 있으며, 150여 편의 학술 논문을 발표했다. 저서로는 『심리학적 트라우마』, 『트라우마와 몸: 감각 운동을 활용한 심리 치료』, 알렉산더 맥팔레인, 라스 뷔새스와 함께 낸 『트라우마 스트레스: 감당하기 힘든 경험이 몸과 마음, 사회에 끼치는 영향』 등이 있다. 뉴욕타임스 베스트셀러인 『몸은 기억한다』는 2014년에 출간한 그의 최신작으로, 트라우마에 의한 뇌 영역의 변화를 설명함으로써 트라우마 스트레스에 관한 통념을 바꾸어 놓았다. 또한 혁신적인 치료를 통해 기능이 떨어진 뇌를 다시 활성화시킬 수 있음을 보여 주었다. 접기
최근작 : <몸은 기억한다> … 총 8종 (모두보기)
제효영 (옮긴이)
저자파일
신간알리미 신청
성균관대학교 유전공학과를 졸업하였으며, 성균관대학교 번역대학원을 졸업하였다. 현재 번역 에이전시 엔터스코리아에서 출판 기획 및 전문 번역가로 활동하고 있다. 옮긴 책으로는 《몸은 기억한다》, 《유전자 임팩트》, 《대유행병의 시대》, 《신종 플루의 진실》, 《메스를 잡다》, 《피부는 인생이다》 등 다수가 있다.
최근작 : <HOW TO BREW 하우 투 브루> … 총 67종 (모두보기)
김현수 (감수)
저자파일
신간알리미 신청
의사로서의 첫 근무지인 김천 소년 교도소에서빈곤과 장애 청소년들의 현실을 배우기 시작했고, 이후 정신과 전문의 자격을 취득하여 청소년, 지역사회 정신보건, 중독, 트라우마, 정신분석 등의 사회 정신의학과 관련된 일을 주로 해오고 있다.
지역에서는 2001년 사는기쁨 신경정신과를 개업하며 빈곤 가족, 노숙, 인터넷 중독증, 은둔형 외톨이, 가출 및 학교폭력 등과 관련한 일에 참여했고, 2011년 명지병원 정신건강의학과로 옮긴 후에는 지역사회 정신보건사업으로 경기도 광역 정신건강복지센터를 맡아 운영하기도 했으며 중앙심리부검센터 등의 설립과 운영에도 관여했다. 현재는 서울시 자살예방센터 센터장 및 서울시 코비드19 심리지원단 단장, 안산 정신건강트라우마센터 운영위원장을 맡고 있다.
2002년 ‘성장학교 별’을 설립하여 지금까지 상처받은 청소년들을 위한 치유형 대안학교 활동에 참여하고 있다. 2005년 이후 프레네 교육학 및 제도적 교육학을 성장학교 별에서 실천하면서 프랑스 및 공교육 교사들과 활발하게 교류하고 있고, 2018년부터는 관계를 위한 심리학 교사연구단을 설립하여 현장 교사들과도 함께하고 있다.
2004년 치유학교 설립과 위기청소년 지원 등의 공로로 ‘청소년보호 대상’을 받았고, 세 번의 ‘복지부장관 표창’과 더불어 14년간의 노숙인 진료로 ‘서울시 표창’을 받기도 했다. 2018년에는 안산 정신건강트라우마센터 및 복지부 중앙심리부검센터 운영 등에 대한 공로로 ‘대한신경정신의학회 환인정신의학 공로상’을 받았고, 2020년에는 도서『요즘 아이들 마음고생의 비밀』로 대한소아청소년정신의학회에서 수여하는 ‘노경선 저작상’을 받기도 했다. 2021년에는 ‘성장학교 별’ 20주년 운영의 공로로 교보재단으로부터 ‘참교육대상’을 수상했다.
저서로는『요즘 아이들 마음고생의 비밀』『코로나로 아이들이 잃은 것들』『공부 상처』『교사 상처』『중2병의 비밀』등이 있다. 역서로는『트라우마 공감학교』『우리는 왜 분노에서 벗어나지 못하는가』등이 있으며, 감수한 책으로『몸은 기억한다』『증상이 아니라 독특함입니다』등이 있다. 접기
최근작 : <코로나가 아이들에게 남긴 상처들>,<가장 외로운 선택>,<요즘 아이들 학급 집단 심리의 비밀> … 총 47종 (모두보기)
출판사 제공 책소개
트라우마는 그대로 몸에 남는다
“트라우마의 기억은 처음 유입된 시점에서 오랜 시간이 지나도 계속해서 영향을 주는 이물질과 같다.” 어쩌다 찔린 작은 파편 하나가 감염을 일으키듯, 그 이물질에 노출된 신체가 보이는 반응은 유입된 이물질 그 자체보다 훨씬 큰 문제가 될 수 있다.
이 본문은 트라우마가 몸에 남는다는 것이 무슨 의미인지 잘 표현하고 있다. 트라우마는 몸에 단순히 남는 정도가 아니라 큰 문제를 만들 수 있다. 몇 년 전, 1994년에 벌어진 지존파 사건에서 살아남은 유일한 생존자의 이야기가 TV에서 방영됐다. 납치된 뒤 강압에 의해 범행 가담까지 했던 그는 20여 년간 악몽 같은 생활을 했는데, 설문지 방식의 트라우마 체크를 해 보니 총점 88점 기준에 78점이 나왔다. 정상인이 25점 미만이라고 하니 상당히 심각한 수준이었다. 그는 항우울제, 공황장애 약 등 일곱 가지 약을 복용하고 있었고, 자궁암과 유방암 등 여러 ... 더보기
북플 bookple
이 책의 마니아가 남긴 글
친구가 남긴 글
내가 남긴 글
평점
분포
9.7
100자평
배송 문의나 욕설 및 인신공격성 글은 상품 페이지에서 노출 제외처리됩니다.
등록
카테고리
스포일러 포함 글 작성 유의사항
구매자 (1)
전체 (3)
공감순
트라우마에 대해서, 그리고 상처에 대해서 이해하고 싶은 사람들 모두에게 추천하고 싶은 책. 현학적인 글이 아니라, 경험과 연구를 따뜻한 어조와 공감어린 시선으로 풀어낸 책. 구매
Shaina 2021-02-15 공감 (1) 댓글 (0)
Thanks to
공감
마이리뷰
트라우마 저작들의 종결자 새창으로 보기
적지 않은 트라우마 저작들을 읽고난 후 본서를 접했다. 정서를 울리는 실제 치유 사례들도 있고 트라우마의 작동과 기능을 뇌생리학적으로 상세히 풀어내어주기도 하지만 무엇보다도 다른 저작들과의 차별성이라면 트라우마 치유를 위한 방법들이 명쾌히 제시되고 있다는 것이다.
[The body keeps the score]라는 영어 제목을 의역해 [몸은 기억한다]라는 제목을 갖게 되었다. 우리의 몸이 트라우마에 어떤 기능을 잃게 되고 어떤 기능이 악화되는지 등을 그리고 있기도 하고 정상적인 상태에서는 우리의 뇌가 쉬고 있을 때 우리 자신의 몸을 감각하고 있는데 트라우마 상태일 때는 해리되어 우리 자신의 몸을 자각하고 있지 못함도 지적하고 있다.
저자가 말하는 트라우마의 많은 문제점들도 알아가야 할 바이겠지만 무엇보다 안구운동 민감소실 및 재처리 요법(EMDR), 뉴로피드백 치료, 내적가족치료, 공동체가 함께하는 연극치료와 음악치료, 맛사지, 요가, 태극권, 무에타이, 무술, 춤 등의 치료가 얼마나 극적인 효과를 불러오는지가 너무도 인상적이었다.
트라우마도 치유의 길이 있는 거라는 것이 그것도 우리 자신의 몸을 통해 가능하다는 것이 다행스러웠다. 그리고 무엇보다 의미있는 타인과의 관계를 통해서 진정으로 치유될 수 있다는 대목은 인상 깊으면서도 안타깝기도 했다. 의미있는 관계, 사람을 통한 치유라는 것이 바란다고 이루어질 수 있는 것은 아닐 것이기에 그저 사람을 만난다고만 이루어지는 것은 아닐 것이기에 안타까웠다.
하지만 트라우마의 치유를 바란다면 또 가족이나 지인의 트라우마를 이해하기 위한 목적에서도 읽어보면 좋을 책이다.
밑줄긋기 ☞
몸은 기억한다 / 베셀 반 데어 콜크 (2)
몸은 기억한다 / 베셀 반 데어 콜크 (1)
- 접기
이하라 2021-03-02 공감(21) 댓글(2)
Thanks to
공감
몸은 기억한다 새창으로 보기 구매
몸은 기억한다
트라우마가 남긴 흔적들
베셀 반 데어 콜코 지음 제효영 옮김 김현수 감수
책은 별점으로 평가하기가 죄송스러울 정도였으나, 소개해준 이에게 경멸을 담아 별 하나를 과감히 뺐다.
수십 년 전의 이야기부터 거슬러가면서 쓰는데, 마치 어제의 이야기처럼 생생하게 나와서, 무서웠다. 오랜 시간 동안 간직하고 있다가 상세하게 풀어쓴 저자의 힘에 반했지만, 개인적인 나로서는 그렇게 살고 싶지 않다. 심지어 전공도서에 가까운 책을 일반인들도 읽을 수 있을 만큼 쉽고 가독력도 좋다.
트라우마에 대해 관심을 가지게 된 계기, 트라우마를 뇌로 바라보기, 애착 문제가 있거나 성폭력 노출된 아동이 성인이 돼서 어떻게 살고 있는지, 그렇다면 트라우마로 인한 흔적은 지울수 없는 상처로 새기면서 살아야 하나?/회복의 방법은 어떻게 될까. 이런 순으로 이야기가 구성되어 있다.
트라우마로 인해 고통받는 사람들을 면밀히 나타내고 있어, 감정을 컨트롤하기 어려워 눈물이 났다. 수많은 곳이 기억해야 할 문장들로 넘쳐났다. 그 중 기억으로 인해 고통을 받고 있다는 대목이 이 책의 모든 것을 말해주는 것 같았다. 기억. 나도 기억으로 인해 고통받고, 엄마도 현실이 아닌 기억으로 고통받고. 기억은 현실을 넘어 고통을 가져온다.
다이애나 포샤의 말을 남기며 책 읽은 소회를 마친다.
[회복력의 바탕은 자신을 사랑해 주고 맞춰 주는 듬직한 사람에게 이해받는다는 느낌에서 찾을 수 있으며, 그 사람의 생각, 가슴속에 자신이 존재한다는 사실을 깨달을 때 얻을 수 있다.]
- 접기
ㅈ 2021-08-11 공감(4) 댓글(0)
Thanks to
공감
트라우마가 남긴 흔적들에 대해 새창으로 보기
이 책은 트라우마로부터 벗어나면서 삶이 건강해질 수 있게 도와줄 수 있는 책이다. 트라우마 치료의 역사와 원리, 사례를 담고 있는 트라우마의 '바이블'이다.
내가 살아가면서 겪어왔던 일들이 나는 트라우마라고 인식하지 못했었다.
그러던 중, 어떤 한 사건들이 문득 떠오르면서 일상 생활에 영향을 줄 때가 있다.
그 때 생각했다. 그것이 나의 트라우마가 아닐까하고.
트라우마의 원인과 치료 방법을 아는 사람은 얼마나 될까? 과연 치료를 할 수 있을까?
p.36-37
나는 보통 의사들이 하는 일을 했다. 내가 이해할 수 있는 한 부분에 집중한 것이다. 바로 톰의 악몽이었다.
…… "그 약을 먹으면 악몽이 사라진다는 건 알고 있었어요. 하지만 그건 내 친구들, 그들의 죽음을 다 헛된 일로 만들어 버리는 거잖아요. 전 베트남에서 죽은 친구들을 위해서 살아 있는 기념비가 되어야 해요."
나는 망연자실했다. 죽은 이들을 향한 충성심은 그가 삶을 버티게 해 준 힘이었다.
- 나는 악몽을 자주 꾸곤 한다. 어떤 꿈은 나의 잠재적 무의식에 잠들어있던 공포를 꺼내와 새로운 꿈을 만들기도 한다. 무섭다. 다신 꾸고 싶지 않지만 계속 반복하곤 한다. 만약 나에게 어떠한 일들이 없었더라면, 어느 부분의 기억이 상실된다면 하는 생각을 해본 적이 있다.
p.57
트라우마는 마음과 뇌가 인지한 정보를 다루는 방식 자체를 근본적으로 재편한다.
우리가 생각하는 방식과 생각하는 것을 바꾸어 놓을 뿐만 아니라 생각하는 능력도 변화시킨다.
p.244
우리 자신을 아는 것, 즉 정체성을 갖기 위해서는 반드시 '현실'이 무엇이고 과거에는 무엇이었는지 알아야 한다(혹은 최소한 자신이 안다는 걸 느낄 수 있어야 한다).
p.518
과거의 일을 현시점에서 신체적으로 다시 경험하며 안전하고 자신을 지지해 주는 존재들로 이루어진 '한정된 공간' 속에서 그 기억을 다시 쓰는 과정은 원래 기억을 보충해 줄 새로운 기억을 만들어 내는 아주 강력한 효과를 발휘한다.
트라우마를 극복하기 위해서는 누구에게나 자신감이 필요하다. 그렇지 않으면 자신이 믿는 것, 지지하는 것, 헌신하고 싶은 것이 무엇인지 주장할 수 있게 해 주는 행위 주체 의식이 발달하지 못한다고 저자는 말한다.
자신이 버려지고, 쓸모없고 존재감도 없는 존재라고 느끼면 어떤 일도 중요하게 느껴지지 않는다. 하지만 트라우마로 인해 나타나는 증상들은 모두 각자가 가진 힘이며 생존하기 위해 터득한 방법이라고 저자는 생각한다.
총 680페이지의 이 책은 사실 읽기가 쉬운 내용은 아니다. 무엇보다 지금 현재 트라우마를 갖고 있는 사람이라면 더욱 힘들 수 있다. 하지만 트라우마가 대체 무엇인지, 그리고 트라우마를 치유하는 것에 있어서 꼭 필요한 책이라 말할 수 있다.
'트라우마가 있나요?' 그럼 주저하지 말고 이 책을 집어주세요.
(가능하다면 모든 사람이 읽었으면 하는 바람의 책입니다.)
무엇보다 중요한 사실은 남들과 함께 있을 때 안심할 수 있어야 정신도 건강하다는 것이며, '관계' 는 의미 있고 만족스러운 삶을 형성한다고 저자는 강조합니다.
그렇게 우리는 어떻게 해야 이 문제에 효과적으로 대처할 수 있는지 잘 알고 있다.
알고 있는 사실대로 행동할 것인지는 이제 우리의 선택에 달려 있다. (저자의 '닫는 글' 마지막 부분에서)
"해당 게시물은 출판사로부터 도서를 제공 받아 작성되었습니다."
- 접기
그대의하루 2020-11-13 공감(4) 댓글(0)
Thanks to
공감
몸은 기억한다 새창으로 보기
"해당 게시물은 출판사로부터 도서를 제공 받아 작성되었습니다."
"끔찍했던 경험은 어떻게해서 당사자가 아무 희망 없이 과거에만 머물러 있도록 만드는 것일까?"
- 본문 내용 중에서
당사자가 아니므로 누군가의 고통의 크기는 함부로 가늠해서는 안 되는 것이다. 그중에서 신체가 아닌 정신적인 고통은 더욱 그러하다. 그리고 우리가 정신적 질병이라 치부하는 대부분의 질병은 몸의 질병을 늘 데리고 온다. 그렇기에 우린 원인을 알 수 없는 가볍지만 끈질기게 우리를 쫓아다니는 질병을 '스트레스'가 원인이 되는 질병이라 말하는지도 모른다. 그중에서 우리가 쉽게 이야기하지만 끈질기게 괴로움의 원인이 되는 것이 '트라우마'가 아닐까 싶다.
많은 사람들에게 익숙하지만, 그만큼이나 많은 사람들이 정확히 알지 못하는 병이 '트라우마'가 아닐까 싶다. 책을 읽기 전 내가 알고 있는 트라우마는 '정신적'인 질병이었다. 하지만, 평생을 트라우마 연구에 바쳐온 저자는 단순히 '정신적'인 질병만이 아니라 말한다. 이는 정신뿐만 아니라 몸이 기억하고 있는 질병이며, 다른 몸의 질병과 동일하게 약물로 치료가 될 수도, 약물이 아닌 다른 방법으로 치유될 수도 있는 병이라 말한다.
이 책은 감히 트라우마의 시작과 끝이 모두 담겨있다 표현하고 싶은 책이다. 트라우마는 아주 큰 사건에서 작게 남기도 하고, 작은 사건에서 크게 남을 수도 있다. 나에게 있는 것이 극복 가능했던 트라우마일 수도 있고, 내가 누군가에게 트라우마를 만든 존재가 될 수도 있다. 그렇기에 한 번쯤은 시간을 들여 읽어보라 추천하고 싶다. 나의 건강한 정신과 몸을 위해, 그리고 타인의 몸과 정신에 함부로 상처를 주지 않기 위해서 말이다.
- 접기
김지영 2020-11-13 공감(1) 댓글(0)
Thanks to
공감
트라우마와 사회에 대한 공부 새창으로 보기
책을 받자마자 깜짝 놀랐습니다.
책의 두께가 무려
3.5cm에 달합니다. 하하.
그런데, 이 책장의 두께가 무색할 만큼
책을 손에서 놓지 못하였습니다.
트라우마는 그대로 몸에 남는다!
트라우마 장애를 안고 있는 사람들은
현재를 살지 못합니다.
그 사건이 일어난 시간에 멈춰
과거 속에 묶인 채
그 일을 반복해서 경험하고 있습니다.
어떻게 트라우마의 굴레에서
벗어날 수 있을까요??
트라우마 연구와 치료 분야에서
가자 뛰어난 선구자 중 한사람이 이룩한
중대한 업적을 이렇게 편히 읽을 수 있다니
개인적인 풍요로움도 느껴집니다.
트라우마에 대한 현대 고전의 바이블!?
한편으론,
심리학 인문서 정도로만 생각했는데,
학문적인 깊이감에
경이로움에 빠져도 보았습니다.
트라우마를 겪는 독자라면
어쩌면
새로운 극복방법의 길을
찾을 수 있을 것 같기도 합니다.
명료하고 흥미진진하며
인상적인 사례들이 가득해서,
트라우마와 관련된 지적수준이
켜켜이 쌓인 느낌입니다.
전문가의 열정과
독자의 호기심이 결합되어
무척이나 재미있었습니다.
명확한 비전과 폭넓은 지혜를 담았고,
의학 분야 전공과는 거리가 먼~~~
제게도 이해하기 쉬운
친절한 설명서 였습니다.
트라우마에 관심이 있는 독자라면
저처럼
책을 내려 놓을 수
없을 겁니다.
트라우마 스트레스를 이해하고 치료하는 일,
트라우마가 사회에 주는 영향에
관심이 있는 사람이라면
추천합니다.
- 접기
은양 2020-10-29 공감(0) 댓글(0)
Thanks to
======
마이리뷰
구매자 (3)
전체 (35)
리뷰쓰기
공감순
트라우마 정보의 종결자
이 책을 읽기 전에 이미 다른 트라우마 저작들을 몇권 읽었었다. 그래서 내가 보다 깊이 느낀 이 책과 다른 트라우마 저작들의 극명한 차별성이라면 이 책은 트라우마를 지닌 이들의 정서에도 물론 주목하지만 그보다는 검증 가능하고 확실한 트라우마 치료법들을 열람할 수 있다는 것이다.
누구나 자신만의 고통이 있다지만 전쟁에 참여해 외상 후 스트레스라는 트라우마를 지니게 된 사람들과 생에 있어 고통을 상쇄할만치의 기쁨과 즐거움이 아직 익숙치도 않을 시절 (뇌의 시스템 전체에 손상을 가져오는, 학대와 방치를 3세까지 경험했거나 더나아가 6세까지 학대와 방치에 노출된) 아동트라우마를 겪는 아이들을 보며 왜 이런 고통이 난무해야하는지 착잡하기 이를데 없었다.
학대나 방치 받은 아이들에게 일어나는 뇌손상은 치료법을 경험하기 전까지는 영구적이며 불가역적인 손상인 것이다.
본서는 외상 후 스트레스, 즉 트라우마 환자들의 뇌를 통해 어떠한 손상이 일어나며 그것이 보편적인 사람들의 뇌와 어떠한 차이를 보이는지 보여준다. 이에 대해 안구운동 민감소실 및 재처리 요법(EMDR), 뉴로피드백 치료, 내적가족치료, 공동체가 함께하는 연극치료와 음악치료, 맛사지, 요가, 태극권, 무에타이, 무술, 춤 등의 치료가 얼마나 극적인 효과를 불러오는지를 전하고 있다.
이 책은 전쟁 후 나타난 외상 후 스트레스 환자들로 부터 시작된 트라우마에 대한 관심과 연구가 재해를 당한 사람들과 일상 속에서 학대와 방치를 당하는 영유아들로 확대되며 연구되어온 역사 그 자체와도 같은 책이다. 트라우마라는 것에 대한 그간의 연구와 성과를 집대성한 책이라 할 수 있다.
트라우마에 빠진 아이들이나 사람들을 보면서 마음 아파하다가 그들이 치유되는 과정에 환호하게 되는 그런 책도 읽어볼만은 할 것이다. 하지만 이 책처럼 트라우마에 빠진 사람들에 대해 이해하게 해 주고 그 치유 가능성과 치유 과정이 어떠리라고 짐작케 해 주는 책은 더욱 가치있는 책이 아닌가 싶다. 가까운 누군가가 트라우마에 빠져 있다거나 본인이나 가족이 트라우마를 치료받기 위해 준비 중이라면 더더욱 읽어보라고 권하고 싶다.
---
트라우마를 경험한 사람들에게는 세상 사람들이 트라우마를 아는 사람과 알지 못하는 사람으로 극명히 나뉜다. 정신적 외상이 된 경험을 해 보지 않은 사람은 그런 일을 이해하지 못하므로 믿을 수 없다고 생각한다. 안타깝게도 그 대상에 배우자나 자녀, 함께 일하는 동료들이 포함되는 경우가 대부분이다.
트라우마 희생자들에게 예전에 겪은 일을 말로 표현하도록 하는 것은 큰 의미가 있고 도움이 되는 것은 사실이지만, 보통 그것만으로는 충분치 않다는 사실도 밝혀졌다. 신체가 자동으로 과도한 경계 태세를 유지하고 언제든 공격이나 폭력을 당할 태세를 갖추며 이에 따라 나타나는 신체와 호르몬 반응을, 당시 이야기를 말하는 것만으로는 바꿀 수 없다. 실질적인 변화를 유도하려면, 위험 요소가 지나갔다는 사실을 신체가 깨닫고 주어진 현실을 살아갈 수 있어야 한다.
사람은 자신이 알고 있는 것을 알지 못하고 자신이 느끼는 것을 느끼지 못하면 결코 나아질 수 없다.
-엘빈 셈라드 교수
기본적인 욕구가 채워지지 않는 사람은, 생각이 아주 고귀하고 세상에 널리 알려진 업적이 아무리 많다하더라도 제대로 발달하지 못한 존재로 남는다.
자기 몸의 상태를 본능적인 욕구 측면까지 모조리 인정할 수 있을 때만 비로소 자신의 삶을 온전히 책임질 수 있다...
단순히 도망갈 기회가 주어진다고 해서 트라우마에 사로잡힌 동물이나 사람이 자유를 찾아가지는 않는다.
... 트라우마에 시달리는 사람들 역시 기회가 주어져도 그냥 포기해 버리는 경우가 많다.
...정신적인 외상을 입은 사람들은 실질적인 위험이 사라지고 오랜 시간이 흐른 뒤에도 계속 다량의 스트레스 호르몬을 분비한다... 외상 후 스트레스 장애 환자에게서 스트레스 호르몬인 코르티솔 수치가 낮게 확인됐다... 코르티솔이 몸에 ‘이제는 안전하니 안심해도 된다‘는 신호를 보내는 역할을 맡아 신체의 스트레스 반응을 종결시킨다... 즉 외상 후 스트레스 장애 환자의 경우 위험 요소가 다 사라진 후에도 체내 스트레스 호르몬이 정상 수준으로 돌아오지 않는 것이다.
스트레스 호르몬이 계속 분비되면서 불안과 공황 상태가 나타나며, 장기적으로는 건강이 사정없이 파괴된다.
반복되는 상황은 오히려 더 많은 고통과 자신에 대한 증오로 이어질뿐이다. 실제로 치료 과정에서 트라우마 경험을 다시 떠올리는 것만으로도 그 일에 관한 생각에 사로 잡히고 집착이 더 강해질 수 있다.
과거 사건의 재현과 재생은 어떤 면에서 트라우마 자체보다 더 큰 악영향을 미친다. 트라우마 사건에는 시작과 끝이 있고, 어떤 식으로든 종결되었다. 그러나 외상 후 스트레스 장애 환자들에게는 그 사건이 깨어 있을 때나 잠을 잘 때나 어느 때고 재현된다. 언제 다시 떠오를지, 얼마나 오래 이어질지 알 수도 없다.
트라우마 구성 요소들이 반복해서 되살아나면, 그로 인해 분비된 스트레스 호르몬이 그 기억을 마음에 훨씬 더 선명하고 깊게 새긴다.
트라우마를 경험한 희생자들에게 그 일을 억지로 이야기하게 하면 혈압이 상승하는 사람도 있고 편두통이 시작되는 사람도 있다. 또 감정적으로 무감각해져 어떠한 변화도 느끼지 못하는 사람들도 있다. 그러나 연구를 해 보면, 공통적으로 심장이 달음박질 하고 스트레스 호르몬이 온몸을 휘젓고 다니는 상태가 예외없이 포착된다.
이와 같은 반응은 앞뒤 없이 불쑥 나타나고 대부분 통제가 불가능하다. 제어가 불가능한 강렬한 충동과 감정은 사람들을 미치게 만든다.
중요한 사실은 뇌의 인지 시스템이 바뀌었다는 점, 그리고 신체 반응에 과거의 흔적이 그대로 담겨 있다는 점이다.
내면에서 일어나고 있는 일을 느끼고, 정확히 밝히고, 확인하는 것이 회복의 첫단계다.
정신적 외상을 입은 사람들이 과거 일을 떠올리게 만드는 자극을 접하면, 우반구는 그 트라우마 상황이 지금 일어난 것처럼 반응한다. 그러나 좌뇌가 적절히 기능하지 못하는 상태라 당사자는 자신의 과거를 다시 경험하고 있으며 과거 일이 재현되고 있다는 사실을 인지하지 못한 채, 그저 격분하거나 겁에 질려 펄펄 뛰고 수치스러워하고 그 자리에 얼어붙어 버린다.
정신적 외상을 입은 사람들은 스트레스 호르몬이 정상 수준으로 돌아오기까지 훨씬 더 오랜 시간이 걸리고, 스트레스를 느끼는 사소한 자극에도 단숨에 불균형적인 수준으로 증가한다. 순식간에 증가한 스트레스 호르몬은 서서히 영향력을 발휘해 기억력과 집중력에 문제가 생기고 쉽게 짜증 나게 만들며 수면 장애의 원인이 되기도 한다. 개인적으로 몸에서 가장 취약한 부분이 어디냐에 따라 장기적으로 수많은 건강 문제를 일으키기도 한다.
...트라우마에 시달리면 특정 상황이 위험한지 안전한지 잘못 해석하는 비율이 높아진다.
트라우마란 ‘영원히 지속되는‘ 상태가 최고조에 이르는 경험이다.
따라서 시상이 망가지면 트라우마가 처음부터 시작, 중간, 끝이 있는 하나의 이야기로 기억되지 않고 당시의 이미지, 소리와 공포, 무기력감 등 어떤 강렬한 감정 상태에서 느낀 신체 감각이 뿔뿔이 흩어진 감각의 흔적으로 기억된다.
머릿속이 멍해지는 증상은 외상 후 스트레스 장애에서 나타나는 대표적인 특성이다... 트라우마가 되살아나면 극적인 변화를 겪고 감짝 놀라 자기 파괴적인 행동까지 할 수도 있지만, 시간이 지나면서 현실감을 잃어버리는 이 같은 변화는 훨씬 더 큰 손상을 가져올 수 있다.
트라우마 스트레스 치료에서는 환자가 과거에 대해 느끼는 감각을 없애버리는 데 중점을 두는 경우가 많다...... 감각을 없애면 반응성을 줄일 수 있겠지만,가만히 길을 걷거나 요리를 하고 아이들과 같이 노는 것과 같은 평범한 일상에서 만족감을 느끼지 못한다면 삶은 그냥 스쳐 자나가 버린다.
정신건강에서 가장 중요한 것을 한가지만 꼽는다면, 다른 사람들과 함께 지내면서 안심하고 살 수 있는 것이라고 할 수 있다. 안전한 유대 관계는 의미있고 만족스러운 삶을 만드는 필수 요소다.... 단지 다른 사람이 존재하기만 하는 상황은 사회적 지지와 다르다.
정신적 외상을 입은 사람들 중 많은 수가 만성적으로 주변 사람들과 잘 지내지 못한다.
트라우마는 싸움 또는 도주 반응으로 표출될 뿐만 아니라 신체 기능이 중단되고 현실에 참여하지 못하는 상태로도 나타난다.
- 접기
이하라 2018-11-17 공감(22) 댓글(0)
Thanks to
공감
트라우마 저작들의 종결자 새창으로 보기
적지 않은 트라우마 저작들을 읽고난 후 본서를 접했다. 정서를 울리는 실제 치유 사례들도 있고 트라우마의 작동과 기능을 뇌생리학적으로 상세히 풀어내어주기도 하지만 무엇보다도 다른 저작들과의 차별성이라면 트라우마 치유를 위한 방법들이 명쾌히 제시되고 있다는 것이다.
[The body keeps the score]라는 영어 제목을 의역해 [몸은 기억한다]라는 제목을 갖게 되었다. 우리의 몸이 트라우마에 어떤 기능을 잃게 되고 어떤 기능이 악화되는지 등을 그리고 있기도 하고 정상적인 상태에서는 우리의 뇌가 쉬고 있을 때 우리 자신의 몸을 감각하고 있는데 트라우마 상태일 때는 해리되어 우리 자신의 몸을 자각하고 있지 못함도 지적하고 있다.
저자가 말하는 트라우마의 많은 문제점들도 알아가야 할 바이겠지만 무엇보다 안구운동 민감소실 및 재처리 요법(EMDR), 뉴로피드백 치료, 내적가족치료, 공동체가 함께하는 연극치료와 음악치료, 맛사지, 요가, 태극권, 무에타이, 무술, 춤 등의 치료가 얼마나 극적인 효과를 불러오는지가 너무도 인상적이었다.
트라우마도 치유의 길이 있는 거라는 것이 그것도 우리 자신의 몸을 통해 가능하다는 것이 다행스러웠다. 그리고 무엇보다 의미있는 타인과의 관계를 통해서 진정으로 치유될 수 있다는 대목은 인상 깊으면서도 안타깝기도 했다. 의미있는 관계, 사람을 통한 치유라는 것이 바란다고 이루어질 수 있는 것은 아닐 것이기에 그저 사람을 만난다고만 이루어지는 것은 아닐 것이기에 안타까웠다.
하지만 트라우마의 치유를 바란다면 또 가족이나 지인의 트라우마를 이해하기 위한 목적에서도 읽어보면 좋을 책이다.
밑줄긋기 ☞
몸은 기억한다 / 베셀 반 데어 콜크 (2)
몸은 기억한다 / 베셀 반 데어 콜크 (1)
- 접기
이하라 2021-03-02 공감(21) 댓글(2)
===
몸은 기억한다
"몸은 진실을 기억한다. 트라우마가 가슴이 터질 것 같은 느낌이나 속이 뒤틀리는 기분으로 몸에 남아 있다면, 가장 먼저 싸움 - 도주 상태에서 벗어나 위험에 대한 인식을 바꾸고 타인과 관계를 형성할 수 있도록 도와주어야 한다"(552)
하나의 이야기처럼 책 한 권을 그대로 읽어내려가다가 문득 '몸은 진실을 기억한다'라는 말에 심장이 쿵 와닿는다. 트라우마라고 하면 커다란 사건이나 지워지지 않는 외상에 대한 것 같은 굵직한 덩어리만을 생각하고 있었는데 그것은 일상적으로 내게도 해당되는 것이기도 하다는 것을 인식하기 시작한 내게 오히려 위안이 되어주고 있다. 언젠가부터 왠지 모를 불안에 빠져있곤 했었는데 어쩌면 그 이유가 어머니의 건강과 관련된 것인지 모른다는 생각이 든 것이다. 어머니가 숨을 멈추고 쓰러졌을 때즈음 내가 인식하기도 전에 악몽에 시달려 비명을 지르기도 했고, 내가 내 비명소리에 놀라 깨기도 했었지만 시간이 흐르면서 괜찮아지고 있다고 생각했었다. 그런데 어머니가 조금이라도 몸이 이상한 것 같은 반응을 보이면 나도 모르게 심장이 뛰고 불안한 느낌이 지속되는 것이었다. 그래서 나는 이 책을 더 읽어보고 싶었다. 트라우마가 남긴 흔적들,이라는 부제도 의미심장하지만 '몸은 기억한다'라는 제목은 나뿐만 아니라 내 주위의 모든이가 나름대로 조금씩은 겪고 있을지 모르는 '트라우마'에 대해 좀 더 접근을 하고 그것을 극복할 수 있는 방법을 찾아보고 싶게 만들고 있다.
책을 읽으면서 노트에 옮겨적은 내용들이 꽤 많다. 그 내용을 살펴보면서 이 책에 대한 요약을 해볼수도 있겠지만 솔직히 그러고 싶지 않다. 이 책을 읽으면서 중반이 넘어갈 때쯤 나는 나 자신의 트라우마에 대한 기억을 떠올리고 내가 주위에서 접해본 외상 후 스트레스장애에 대한 - 사실 어떤 관점에서 보자면 별 것 아니라고 여길수도 있는 그런 가벼운 이야기들에 대해서 좀 더 관심이 집중되었기 때문이다. 우선은 나 자신에 대한 것을 알고 난 후 다시 읽어볼 때에는 다른 이들의 트라우마에 대해 깊이있는 파고들기를 해봐야겠다는 생각을 하게 되었기 때문이기도 하고.
약물치료나 역할극을 하는 치유과정에 대해서는 트라우마에 대한 특별한 관심이 없다하더라도 다들 한번쯤은 들어서 알고 있는 내용일것이다. 여러가지 사례에 대해서는 무척 흥미롭게 읽을 수 있었는데 솔직히 말하자면 뇌파에 대한 이야기들은 그림과 사진을 보면서 대략적으로 훑어지나가버려서 내가 이 책을 완전히 이해했다고는 할 수 없다.
다만 한 사람을 이해하려면 그 사람의 과거에 대해 아는 것이 많은 도움이 된다는 것을 이 책을 읽으며 확신하게 되었고, 그것은 단지 이해하기 위한 것으로 끝나는 것이 아니라 그 사람의 미래가 좀 더 평화로운 마음으로 살아가는 삶이 될 수 있도록 도움을 주기 위해서 무엇인가를 시도해 볼 수 있으며, 그 무엇인가를 찾기 위한 첫번째 노력은 어쩌면 이 책을 읽는 것에서부터 이미 시작된 것일지도 모른다는 생각을 하게 되었다.
이 책의 시작은 그리 재미있지는 않다. 지금은 자연스럽게 떠올리게 되고 이해하고 있지만 백여년 전을 떠올려본다면 트라우마로 인한 고통을 겪는 이들에 대한 이해는 물론 과거의 상처로 인해 성인이 되어서 불안정한 삶을 살아가고 있는 이들에 대한 이해도 없었던 시대가 있었음을 생각하게 된다. 그 후 전쟁, 홀로코스트 같은 커다란 사건뿐만 아니라 가정폭력, 성폭행 같은 개인의 아픈 상처 역시 뇌에 각인되어 무의식중에 그 상처를 드러내고 있음을 많은 연구자들에 의해 알게 된 것이다. 그리고 그러한 트라우마는 결코 치유될 수 없는 것이 아니라 고통을 극복하고 자신과 화해하며 더불어 살아갈 수 있는 상처임을 새삼 깨닫게 하고 있다.
누구에게나 저마다의 삶의 고통을 다 갖고 있다,라는 생각에 모두 동의할 것이다. 그렇지만 그 고통속에 자신을 파묻어버리고 살아갈 것인지, 변화하기 위해 마음을 열고 자신의 내적 경험을 받아들이며 자기 자신을 통제하고 자기 스스로를 자각하며 트라우마와 직면하여 이겨내려 노력하며 다른 시각과 다른 마음가짐으로 바라보는 다른 세상을 살아갈 것인지, 그것은 스스로의 선택이 될 것이다. 물론 혼자가 힘들다면 주위의 도움을 받을수도 있고, 전문의의 도움과 때로 누군가는 약물의 도움을 받는 것도 도움이 될 수 있다.
"트라우마는 자신의 나약함과 끊임없이 대면하게 만든다. 또한 인간이 다른 인간에게 가하는 비인간적인 행위에 대처하도록 만들지만, 동시에 월등한 회복 능력을 발휘하게 한다. ... 수많은 사람이 그 고통스러운 경험에도 불구하고 누군가의 소중한 파트너가 되고 부모가 되며 모범적인 선생님, 간호사, 과학자, 예술가로 살아간다"(563)
이 책의 모든 부분이 다 인상적이고 마음을 움직이고 있지만 특히 닫는 글의 마지막 문장은 더 마음을 울리고 있다. "공중보건 분야에서 현재 가장 시급한 문제는 트라우마이고 우리는 어떻게 해야 이 문제에 효과적으로 대처할 수 있는지 잘 알고 있다. 알고 있는 사실대로 행동할 것인지는 이제 우리의 선택에 달려있다"
- 접기
chika 2016-02-13 공감(10) 댓글(0)
Thanks to
공감
몸은 기억한다 새창으로 보기
#트라우마 에 몰입되다. 내 몸엔 어떤 기억들이 담겨져 왔을까.... 겨울호랑이님을 통해 연을 맺을 뻔한 책이 이제사 내 손에. 신의입자를 다 읽어내긴 무리였는지 두통이 ㅠㅠ 생소한 물리학 양자역학은 이제 편독의 대상이 될 수밖에 없는 건가. 그래도 욕심은 안 생기니 다행이다. 이 책도 신...에 만만치 않게 좋은 책이다. 나는 나의 직관을 믿는다.
고백한다. 이 책을 읽으면서 여러 차례 눈물을 훔쳤다. 나 자신의 개인적 트라우마를 건드릴 뿐 아니라 세월호, 위안부 등 지금 당면한 우리들의 트라우마를 어떻게 다가서야 하는지를 깨닫게 해 주었기 때문이다. 5p
- 감수 및 추천의 말 중에서
- 접기
:Dora 2017-03-14 공감(9) 댓글(0)
Thanks to
공감
[마이리뷰] 몸은 기억한다 새창으로 보기
모든 기억에 이러한 두 가지 특성이 있다니 이상한 일이다. 그 기억들은 항상 너무 고요하기만 한데, 그 점이
가장 놀랍다. 심지어 현실에서 일어날 것 같지 않은 일들도 그런 특징을 똑같이 갖고 있는 듯하다. 소리 없는
환영처럼, 아무 말 없이 고요한 가운데
내게 모습과 몸짓으로 말을 건다.
나를 괴롭히는 건 바로 그 고요함이다.
- 에리히 마리아 레마르크
회복력의 바탕은 자신을 사랑해 주고
맞춰 주는 듬직한 사람에게 이해받는다
는 느낌에서 찾을 수 있으며, 그 사람의
생각, 가슴속에 자신이 존재한다는 사실
을 깨달을 때 얻을 수 있다.
-다이애나 포샤
누구에게나 크고 작은 트라우마가 있다
고 생각한다. 그것을 극복하느냐 못하느냐에 따라서 삶은 정반대로 진행
되기도 한다. 세월호부터 포항 지진에 이르기까지 트라우마는 진행형이고 앞으로도 일어날 일이다.
이 책은 트라우마에 대한 바이블이라 할
수 있다. 트라우마 치료의 역사,원리 그리고 사례와 트라우마를 다루는 사회
의 철학과 방향까지 모두 담겨 있다.
이례적으로 포항 지진으로 인해 수능이
연기 되었다. 일부 이기적인 학생들이
sns에서 포항수험생들에게 책임을 따지며 욕설한다는 기사를 보면서 백번
을 참고 이해한다면 속상해서라고 친다.
그러나 천재지변의 당사자인 포항 수험
생들을 보듬어 주는 수험생들이 대다수
일 것이라고 생각하고 싶다.
사람의 결속과 친화는 좋은 일속에서 보다는 나쁜 일속에서 더 잘 된다.
위기를 기회로
모든 수험생들이 오히려 일주일 시간을
더 벌었다는 긍정적인 마인드로 23일
치룰 수능에서 원하는 성적보다 더 잘
나오기를 빌어본다.
그래서 하나의 트라우마는 지우시기를.
.....
- 접기
우민(愚民)ngs01 2017-11-18 공감(7) 댓글(1)
Thanks to
공감